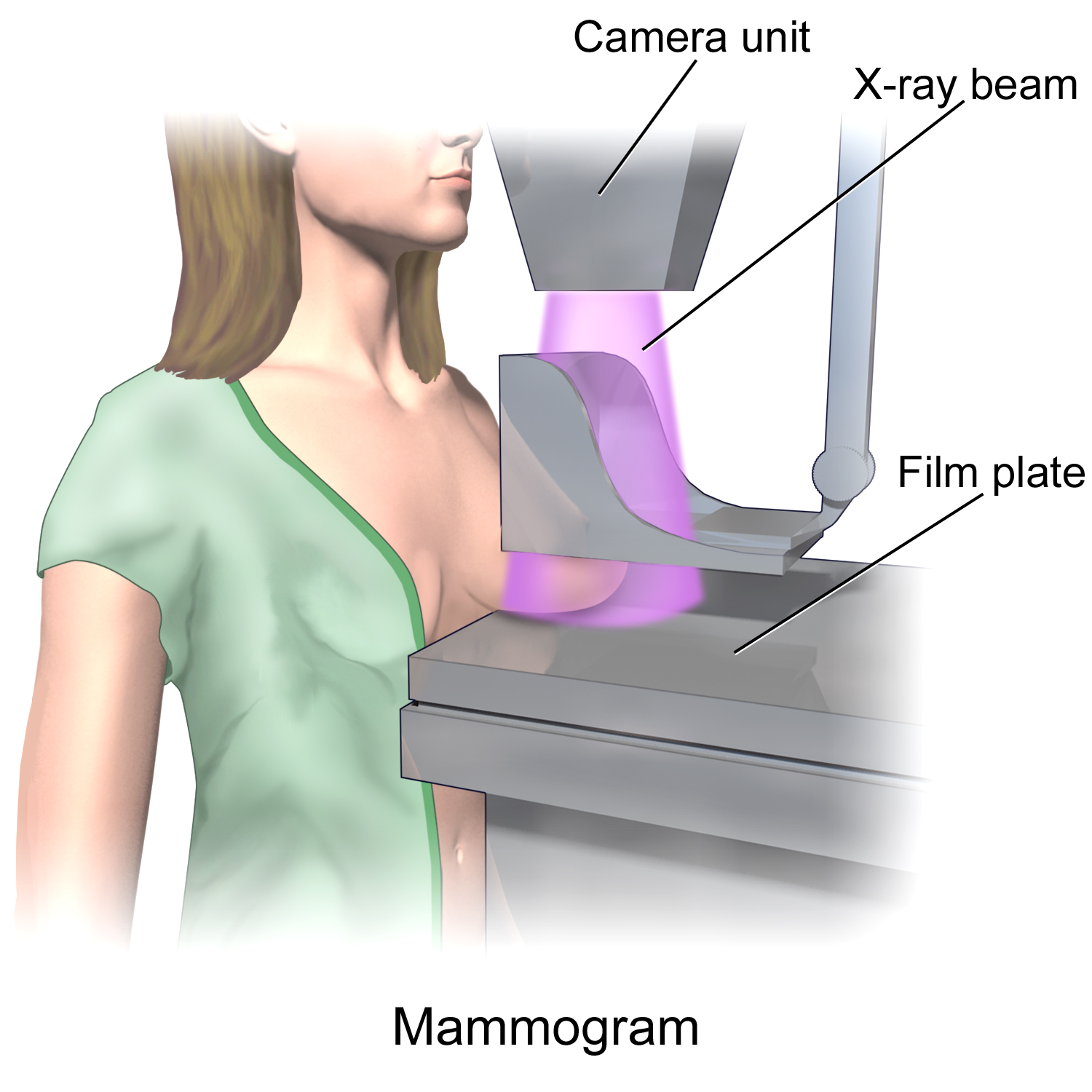
Women have difficult decisions to make regarding mammograms. Medical organizations are providing conflicting opinions as to the best age to start a mammogram and how often to get them. Recently the American Cancer Society changed its recommendations. It now suggests women of average cancer risk begin at age 45 rather than age 40 and then get a repeat mammogram every two years instead of one. The organization also said that it does not think a doctor's manual breast exam is very helpful. Many doctors have decided to ignore these changes and continue to suggest the yearly mammograms. But what is the downside to getting these tests earlier and more often? Isn't it better to catch a tumor early through frequent tests?
 We have had many emails this week asking my opinion regarding these changes. Long term readers of my newsletter have previously read that I actually recommended these less stringent guidelines many years ago. I recognized the harm that more frequent testing can cause could outweigh the benefits.
We have had many emails this week asking my opinion regarding these changes. Long term readers of my newsletter have previously read that I actually recommended these less stringent guidelines many years ago. I recognized the harm that more frequent testing can cause could outweigh the benefits.
Women with a personal history of breast cancer, a family history of breast cancer, a genetic mutation known to increase risk of breast cancer (such as BRCA), and women who had radiation therapy to the chest before the age of 30 are at higher risk for breast cancer, and may consider earlier and more frequent mammograms. However, women of average risk, in my opinion, are better off starting at age 45 rather than 40. I list my reasons below:
Potential harm from mammograms
We all know the benefits of early detection of a breast tumor and subsequent effective treatment before it metastasizes. However, few women know about the risks and potential harm from aggressive testing, much having to do with false-positive results. A false positive is when the mammogram says that there may be a tumor there but further testing, such as a biopsy, shows nothing is there.
It is estimated that a woman who has yearly mammograms between ages 40 and 49 has about a 30 percent chance of having a false-positive mammogram at some point in that decade and about a 10 percent chance of having a breast biopsy within the 10-year period. About 80% of all breast biopsies result in benign (no cancer present) findings. The radiologist may notice something unusual on the mammogram, and due to the fear of being sued, will suggest a biopsy even though it may not be necessary. Doctors are so afraid of missing a potential tumor that they will send their patients with minor abnormalities for additional testing even though they may not be needed thus significantly increasing the rate of false positives and further x-rays, blood tests, and other diagnostic procedures.
Screening mammography, like all cancer screening tests, has potential drawbacks, including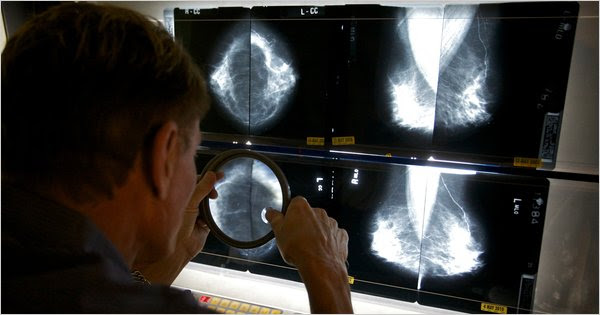 adverse effects on survival, comfort, function and psychological well-being emanating from all procedures that result from screening. Since the average risk of dying from cancer during the 40s is relatively low, 1,900 women in that age group would need to be screened for a decade, and suffer anxiety and all kinds of emotional, financial, and other hardships, to PERHAPS increasing life expectancy of one life.
adverse effects on survival, comfort, function and psychological well-being emanating from all procedures that result from screening. Since the average risk of dying from cancer during the 40s is relatively low, 1,900 women in that age group would need to be screened for a decade, and suffer anxiety and all kinds of emotional, financial, and other hardships, to PERHAPS increasing life expectancy of one life.
More reasons why testing in not as safe or beneficial as some doctors claim are explained athttp://www.raysahelian.com/